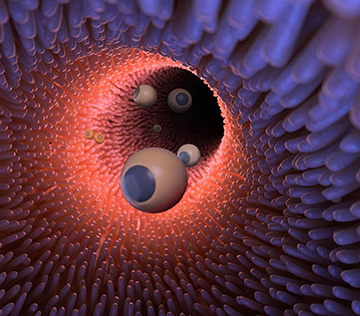
An artist’s illustration of self-propelled, photoacoustic-tomography-tracked microrobots inside the gut. [Image: Caltech]
The use of micro- and nanoparticles for targeted drug delivery and therapeutics has stoked considerable excitement and progress. But just how to image and activate those tiny warriors at depth in a patient’s body remains a tough problem.
To tackle that problem, a U.S. research team has now developed a prototype system of self-propelled, drug-laced “microrobots” to deliver therapeutics to cancerous intestinal tissue. At the heart of the system is a light-based technique, photoacoustic tomography, that’s used to track the bots deep in the organism and then set them loose when they reach the neighborhood of a tumor (Sci. Robot., doi: 10.1126/scirobotics.aax0613).
Drug-delivering micro-rockets
To create the system, the research team, led by Wei Gao and OSA Fellow Lihong Wang of the California Institute of Technology (Caltech), began by building up, layer by layer, the micro-bots themselves. At the core of these bots, or micromotors, are commercially purchased magnesium microspheres approximately 20 μm in diameter. In the lab, the team spread these microparticles on a glass slide, and then used a number of chemical-washing and evaporative techniques to coat the spheres successively in a 100-nm-thick layer of gold, an alginate hydrogel layer that embeds a drug (in this case, doxorubicin), and a capping, stability-enhancing polymer layer that can stand up to intestinal acids.
By design, the process for building up the layered microspheres on top of a glass slide leaves a tiny, roughly 2-μm-diameter opening in the applied layers, exposing the magnesium core. That “porthole” is the key to the microparticles’ self-propulsion capabilities. When the magnesium is exposed to intestinal acids through the porthole, it reacts with them, creating a stream of bubbles that jet out of the porthole like gases from a rocket nozzle. The bubble stream propels the microsphere forward until it strikes the surrounding tissue.
Photoacoustic guidance
The team used an emulsion method to package a number of the micromotors into a gelatin solution and then encapsulate them in a paraffin coating—like buckshot in a shotgun shell. The researchers now had a potentially ingestible capsule packed with drug-delivering micro-bots. But how could the team be sure that the bots reached the right place—and set them loose when they got there?
A possible answer lay in photoacoustic tomography (PAT), an emerging technique for deep-tissue imaging that leverages both optical and acoustic energy. In a typical PAT scheme, a short infrared laser pulse, capable of penetrating deep into tissue without causing damage, is absorbed by cells in the body; the absorbed energy is then re-released as heat, which gives rise to a pressure increase that propagates as a photoacoustic wave. That acoustic-wave signal, in turn, can be picked up outside of the body using ultrasound transducers, and computer-processed into images of often striking detail and resolution (see “Multiscale Photoacoustic Tomography,” OPN, April 2018).
Under the Caltech-led team’s approach, the microrobot-containing capsules, once ingested, are imaged and tracked in the patient’s digestive tract using PAT. The wavelength of the PAT-exciting infrared radiation, 750 nm, was carefully chosen to allow the researchers to distinguish between the photoacoustic response of the gold-coated micro-bots, the paraffin capsules, and the surrounding red blood cells.
Then, when the PAT imaging indicates that the bot-containing capsules have reached the vicinity of an intestinal tumor—also imaged using PAT—the area is zapped with an externally delivered, high-power burst of continuous-wave infrared laser energy, which also penetrates into tissues at depth. When tickled by that energy, the gold coating on the encapsulated microparticles, which strongly absorbs infrared radiation, heats up and causes the surrounding paraffin capsule to melt—releasing the micro-bots. That put the magnesium exposed in each bot’s tiny porthole into contact with intestinal fluids, activating the micromotor and rocketing the drug-containing micro-bot toward the intestinal wall, to embed itself in the tumor and deliver the therapeutics.
A Caltech video illustrated the system concept:
From mice to human patients
The team tested the system in model blood vessels embedded in chicken breasts, and also in live mice, and found that it did indeed work to target delivery of the drug-containing particles to the right spot. The researchers also assessed the potential toxicity of the microparticles—both qualitatively, by looking for signs of distress in the treated lab animals, and quantitatively, by comparing body-weight changes of treated and control animals. They found “no significant difference” between the treated and control groups, as well as no evidence of inflammation.
While the trials with lab mice are encouraging, making the system ready for human patients raises some challenges. The biggest is that human treatments could require penetration of tens of centimeters of tissue, substantially more than in a mouse model—and PAT’s tissue penetration is limited by photon dissipation to only around 7 cm. The team believes this hurdle could be overcome by adapting the system to thermoacoustic tomography, an approach analogous to PAT that uses longer-wavelength, microwave radiation to excite the acoustic response.
The team, which in addition to Caltech scientists included researchers from the Washington University of St. Louis, USA, is now at work to move the system closer to something suitable for the clinic, to explore the possibility of its use in tissues other than the intestine, and to determine just how effective the drug delivery can be. “We demonstrated the concept that you can reach the diseased area and activate the microrobots,” Gao, the team co-leader, said in a press release accompanying the work. “The next step is evaluating the therapeutic effect of them.”
