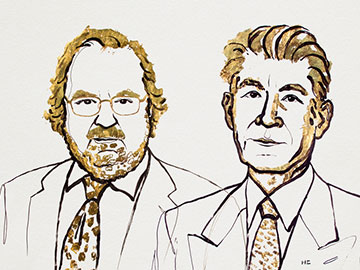
James P. Allison (left) and Tasuku Honjo (right) received the 2018 Nobel Prize in Physiology or Medicine for their path-breaking work in cancer immunotherapy. Some researchers are working on the use of optogenetic techniques for remote control of immune responses, to improve the clinical effectiveness of those therapies. [Image: Illustration by Niklas Elmehed; © Nobel Media AB 2018]
This year’s Nobel Prize in Physiology or Medicine went to two pioneers of cancer immunotherapy, James P. Allison of the M.D. Anderson Cancer Center, USA, and Tasuku Honjo, Kyoto University, Japan. The laureates received their award for their groundbreaking work in “checkpoint” immunotherapy—work that, according to the Nobel Committee, opened an entirely new pathway for treatment of a variety of cancers that heretofore have stubbornly resisted other therapies.
That new pathway could, at least partly, be marked with light. A number of researchers in the past several years have looked at how the techniques of optogenetics, a discipline usually associated with neuroscience, might be used to tune and improve the effectiveness of the cancer immunotherapies whose pioneers were honored this year in Stockholm.
Releasing the brakes
The checkpoint-immunotherapy work honored in the 2018 Physiology or Medicine Nobel focuses on improving the immune system’s reaction against tumors by blocking certain proteins that act as “brakes” on the immune system’s T-cell response. The function of these brakes is to distinguish “self” from “non-self,” so that the immune system only targets invading pathogens. But, unfortunately, tumors also benefit from the protection against immune reactions that these braking proteins confer.
In work begun during the 1990s, the research groups of the two 2018 Nobel laureates performed antibody-based experiments in mice that blocked the impact of two particular braking proteins—CTLA–4 in the case of Allison’s team, and PD–1 for Honjo’s group. Both sets of experiments showed stunning results. By eliminating the immune-suppressing action of the braking proteins and, in effect, turning the immune system loose on the cancers, the blockade prevented or dramatically shrank tumors of malignant melanoma in the lab animals. Subsequent experiments with PD–1 showed that the therapy was effective in other types of stubborn cancers as well.
By the early 2010s, both CTLA–4 and PD–1 therapy had passed through clinical trials, and both are now in use—either alone or in combination with other therapies—in cases of difficult-to-treat cancers. While side effects, particularly autoimmune reactions, can be significant, Anna Wedell of the Karolinska Institute, Sweden, speaking at the Nobel Prize press conference, called the advent of immunotherapy “a completely new tool to add to the toolbox” in treating cancers. “It has revitalized the whole area.”
A role for optogenetics?
As part of that new ferment, some researchers believe that optogenetics—the use of light to control the activity of certain photosensitive genes in vivo—might eventually play a role in boosting the effectiveness of cancer immunotherapy.
Heretofore, optogenetics has been associated principally with neuroscience research in lab animals. In a review article in early 2017, however, Gang Han of the University of Massachusetts Medical School, USA, and Yubin Zhou and colleagues of Texas A&M University, USA, noted that optogenetic techniques might also find a place in cancer immunotherapy. The light-based techniques, they suggested, could allow “remote control” of immune responses within the body. That control would come via photoactivation of T-cell receptors or cell-membrane calcium channels (which modulate immune-cell signaling) that had been genetically altered to respond to light.
A route to fewer side effects
One obvious advantage to such a system is that it could allow the immunotherapy to be closely targeted to the vicinity of the tumor. That, in turn, could reduce the risks of the autoimmune side-effects that represent a key drawback of current immunotherapies. In their review article, Han, Zhou and colleagues dubbed the approach “optoimmunoengineering,” calling it “a nascent but rapidly growing field that requires multidisciplinary efforts from engineers, nanomaterial chemists, immunologists, and cancer biologists.”
In making optoimmunoengineering work, a key issue will be how to deliver light to deeply buried immune cells and tumors. Han, Zhou and their coauthors suggest that leveraging the techniques of so-called wireless optogenetics (via wirelessly enabled micro-LED implants) or using upconversion nanoparticles (UCNPs) to deliver light directly to tumors could provide promising avenues. In work published in early this year, for example, researchers used UCNPs to deliver blue light deep within the brains of live mice for optogenetic activation.
![]()
One possible route to delivering light to tumors could be via wirelessly actuated micro-LEDs, such as these devices designed for neuroscience work by John Rogers and colleagues. [Image: J. Rogers/Northwestern University]
Micro-LEDs
Meanwhile, in experiments published in mid-2017, Minsoo Kim and colleagues at the University of Rochester, USA, and the Gwangju Institute of Science and Technology and Sungkyunkwan University, Korea, explored using micro-LEDs as a light source for optogenetically souped-up immunotherapy. The group infused T cells, which had been genetically modified to express the light-sensitive protein channelrhodopsin, into a melanoma-carrying strain of mice.
The researchers then used an implanted micro-LED device in the mice, glued onto the tumor, to shine wirelesly activated blue light on the modified T cells. The light served as a “control knob” on the cells’ membrane calcium channels that, the researchers found, could be used to substantially improve the effectiveness of immune cells in fighting the cancer—at least in mice.
Clearly, there is a long way to go before optogenetic techniques become a mainstream part of cancer immunotherapy. But the recent work does suggest a potential role for light as an arrow in the quiver—and highlights, more generally, the remarkable potential of the accomplishments honored in this year’s Nobel Prize for Physiology or Medicine.
