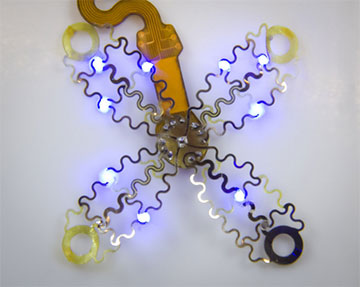
A new optogenetic pacemaker design that envelops the heart. The wireless, battery-free device could be implanted with a less invasive procedure than currently possible and would cause patients less pain. [Image: P. Gutruff]
Pacemakers save lives by detecting heart arrhythmias and correcting them with an electrical jolt. Unfortunately, the electric signal hits pain receptors in addition to heart muscle cells, or cardiomyocytes, causing the patient extreme discomfort. Now, engineers from three US universities are developing an optogenetic pacemaker that may improve the quality of life of patients with heart arrhythmias by using light instead of electricity to signal cardiomyocytes to contract, thereby bypassing pain receptors completely (Sci. Adv., doi: 10.1126/sciadv.abq7469).
The new pacemaker design includes four petal-shaped panels that wrap around the heart and an integrated computer that records heartbeat data and stores algorithms for correcting a variety of heart arrhythmias. The device also functions without wires and batteries by using wireless charging for optical signal delivery and data recording, and it employs an infrared link to upload algorithms to the onboard processor.
The proof-of-concept design was successfully demonstrated in vitro and in freely moving mice with genetically modified cardiomyocytes that contract when exposed to light.
LED stimulation and onboard computing

An artist's rendering shows how a new pacemaker is able to envelop the heart. [Image: P. Gutruff]
The engineers—from the University of Arizona, George Washington University and Northwestern University—designed the new pacemaker’s “petals” from a thin and flexible mesh digitally manufactured from ultrathin layers of polyamide, titanium, silver and platinum. The mesh carries energy to power the signals from microscale inorganic LEDs. A small integrated computer coordinates these light signals per algorithms received via a wireless infrared uplink.
Unlike standard pacemakers that deliver one type of signal, the optogenetic pacemaker can use different algorithms to deliver specific and choreographed pulses of light to treat a variety of heart arrhythmias—for example, synchronizing the contractions of the upper and lower chambers of the heart that go awry during atrial fibrillation.
Electrodes on the optogenetic pacemaker’s mesh petals can collect heart rhythm data during correction because light from the LEDs does not interrupt the recording. This extra data can help physicians gain a better understanding of their cardiac patients’ arrhythmic episodes.
The stimulation, computation and recording components of the optogenetic pacemaker are all powered wirelessly, eliminating the need for batteries that have to be replaced every five to seven years.
Prototype demonstrations
The researchers successfully demonstrated the optogenetic pacemaker prototypes in vitro using mouse cardiomyocytes that were genetically modified to express Channelrhodopsin-2 (ChR2), a protein commonly used in optogenetics that acts as a light-gated ion channel. They also tested it in vivo using mice that were genetically modified to express ChR2. The team found that the device’s onboard computer managed optogenetic stimulation of ChR2-expressing cardiomyocytes with millisecond precision, and that the optogenetic activation area was about 28 mm2 for each of the nine LEDs in the mesh petals.
“These new devices can do much more precise targeting, making defibrillation both more effective and less painful,” said Igor Efimov of Northwestern University. “This technology could make life easier for patients all over the world, while also helping scientists and physicians learn more about how to monitor and treat the disease.”
