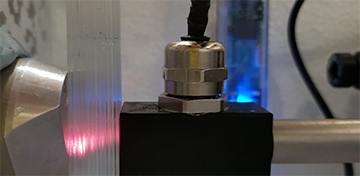
A lung phantom setup showing capillary array and GASMAS probes. [Image: Courtesy of A. Pacheco, TNI.]
Measuring the lungs’ respiratory volume is important for assessing a patient’s condition and diagnosing a number of diseases that obstruct airways. The current approaches to measuring lung volume, however, don’t provide information about local volume changes within the lung—and are difficult to use with newborn infants or patients under anesthesia.
To overcome these limitations, scientists in Ireland have tested an optical method called gas in scattering media absorption spectroscopy (GASMAS)—using not a real lung, but a lung tissue model, or “phantom” (J. Biomed. Opt., doi: 10.1117/1.JBO.27.7.074707). The artificial phantom allowed the scientists to measure volume changes during a respiratory process—thereby demonstrating, according to the study authors, GASMAS’s potential in the clinic.
From bouncing light to gas concentration
A complicated structure of muscles and other tissues, the human respiratory system plays many essential roles, including inhaling oxygen-containing air and exhaling carbon dioxide, and delivering oxygen to cells. Timely detection of any system malfunction is important.
However, detection isn’t always easy. Previously developed methods, such as spirometry and plethysmography, require that patients actively breathe in and out during the test. That makes the tests undesirable for newborn babies or for patients (such as those under general anesthesia) who are unconscious.
Andrea Pacheco of Tyndall National Institute and University College Cork, Ireland, and her colleagues wanted to see if the GASMAS technique could get past these problems, by measuring gas-volume changes in the lungs indirectly based on optical-scattering and absorption characteristics. Not only is GASMAS noninvasive but it can distinguish the absorption signals of gases against the backdrop of signals from organs surrounding the lungs.
The team used two different light sources for the experiment: 760 nm for the absorption band of O2 and 820 or 935 nm for the H2O. Because the concentration of H2O is known (as the relative humidity inside the human respiratory system is kept at 100%), by measuring the intensity of the scattered light, the team could calculate the path length of the light using the Beer-Lambert equation. And by plugging that calculated path length back into the equation with the intensities of light signals for O2, the team could find out the concentration of O2 as well.
A better phantom
While the feasibility of GASMAS had been previously demonstrated in babies, to further improve the method, it had to be tested on non-human subjects. That is where the tissue phantom comes in. Pacheco and colleagues previously built an entire chest region of a newborn baby using various optical phantoms, to test the feasibility of GASMAS on human body. But that model did not account for the lung’s anatomy at the scale of the alveoli—the tiny air sacs at which the exchange of oxygen and carbon dioxide into the blood actually takes place—and, thus, couldn’t nail down how accurately GASMAS might be able to pick up breathing-volume changes in the lungs.
For the new study, the team built a phantom with a capillary structure that matches the size of the alveoli in human lungs. They also used a so-called liquid optical phantom—a mixture of fatty liquid, ink and water—that matches the absorption and scattering properties of lung tissue.
Testing the system
To imitate exhaling, the scientists filled up 20 out of 229 capillaries at each step with the liquid phantom and measured the scattered light signal in each step. The empty capillaries without liquid mimicked the response of the air-filled alveoli. After eleven measurements, including the measurement of the completely empty capillary system, the scientists reversed the process to copy inhaling while performing the same measurements. During the experiment, the entire structure resided in a chamber that maintained the physiologically relevant temperature and humidity.
The team then compared the GASMAS absorption signal with the proportion of air-filled versus liquid-phantom-filled capillaries—and found that the signal steadily declined as the proportion of air-filled capillaries decreased. When Pacheco and colleagues analyzed the data, they realized that they had successfully demonstrated that GASMAS can indeed be used to measure the volume change of the phantom system—and, therefore, of human lungs.
The previous papers on GASMAS “have been more focused in measuring the gas concentration,” Pacheco says. “We show that GASMAS can be used to sense small changes of volume in the phantom. … From there, [we can] try to … design experiments to see if we can somehow use these results and plan a new set of measurements in real patients.”
Phantoms to humans
Using GASMAS on human patients isn’t just a pipe dream. Working in collaboration with INFANT Research Centre in Cork, Ireland, and GPX Medical, a medical device company based in Sweden, Pacheco says she and her colleagues have undertaken an observational study of its use with 100 full-term infants, using a clinical prototype instrument developed by GPX. The team successfully demonstrated the system’s use on their first human patient—a baby—on 1 November.
“The technique has been evolved a lot,” Pacheco says. She adds that there are still more ways that GASMAS can be used, such as in adult patients and with pulmonary endoscope. It may also be used for diagnosing sinus and ear infections. “I see a lot of potential of the technology, but there's still a long way to go,” she says. “But it's just exciting to see that it is feasible to measure … changes in [gas] volume.”
Correction, 16 November 2021, 13:00 EST: This story has been updated to reflect that devices using the GASMAS technique has not yet been approved for clinical use, and to clarify the participants in the observational clinical study described in the text.
Correction, 29 November 2021, 10:00 EST: This story has been updated to clarify that the feasibility of GASMAS on babies had been tested before, and that spirometry and plethysmography are possible on babies, though undesirable.
