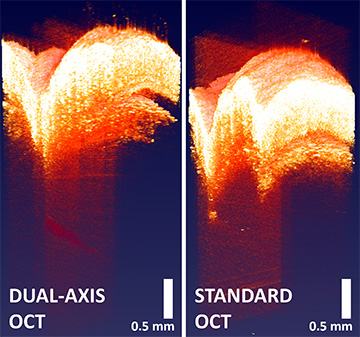
The dual-axis OCT image on the left displays the tip of a needle more than 1 mm beneath a mouse’s skin. In contrast, the standard OCT image on the right fails to do so. “The needle’s highly reflective and scattering,” Jelly says, so being able to clearly see the tip of the needle is “pretty significant.” [Image: Evan Jelly]
Since its debut in 1991, optical coherence tomography (OCT) has gained popularity in medical fields, especially in ophthalmology and optometry. But one limitation of this noninvasive method for imaging living tissues is its shallow detection depth—around 1 mm.
In a new study built on previous research, biomedical engineers in the United States validated an improved OCT method called dual-axis OCT, or DA-OCT (Biomed. Opt. Express, doi: 10.1364/BOE.438621). Specifically, they demonstrated that, by tilting the light source and detector, DA-OCT increases the depth of detection by 50% compared with regular OCT. The engineers expect this enhanced depth to be especially useful in dermatology, as biological processes of interest often occur around 2 to 3 mm below the skin.
Too shallow for skin
OCT relies on backscattered light to image features lying beneath biological tissues. By focusing on target layers, the technique enables cross-sectional images and provides resolution near the diffraction limit without damaging tissue.
Despite widespread interest across medicine, the actual use of OCT has been mostly concentrated in ophthalmology and optometry—ophthalmologists, for example, routinely deploy OCT to assess and treat retinal conditions. This narrow application range traces partly to OCT’s limited depth of detection; its imaging depth of 0.5 to 1.2 mm for 1300-nm light is insufficient for some fields.
Especially in dermatology, “being able to use OCT even 2 or 3 millimeters into the skin is extremely useful because there are a lot of biological processes happening at that depth that can be indicative of diseases like skin cancer,” said Adam Wax, a biomedical engineer at Duke University, USA, and the new paper’s senior author, in a press release accompanying the research.
“Your eye’s designed to accept light and your skin’s designed to reject light,” Evan Jelly, the first author of the paper, also at Duke, told OPN. “So, penetration and depth [are] very challenging, particularly for skin.”
Improving OCT
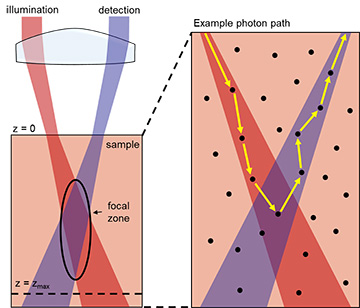
In DA-OCT, both the illumination and detection happen at a slight angle, which increases the imaging depth. [Image: Modified from Matthews et al. Optica 1, 105 (2014)] [Enlarge image]
To improve the imaging depth of OCT, Wax’s group previously developed DA-OCT, introducing a beam of light and a detector at a slight angle of 3 degrees. But while a 2017 Optics Letters paper demonstrated the technique’s feasibility, it didn’t make an “oranges to oranges direct comparison” to the conventional OCT, Jelly says.
In this new study, Jelly and his colleagues deployed both DA-OCT and conventional OCT using 1300-nm light on the same samples—artificial tissues and hairless mice. After collecting images using the two methods, the images from each were fused together using an algorithm to create a 3D image. When the engineers compared the images from DA-OCT with those from conventional OCT, they discovered that DA-OCT could achieve an imaging depth of 2 mm, with a comparable resolution to that of conventional OCT.
Clinical future
Jelly cautions the team’s results don’t mean that DA-OCT is always superior to conventional OCT. “We’re not promising that [DA-OCT] will always go deeper,” he says. “But under certain conditions—and we tried to describe those conditions in the paper—this can outperform or can help resolve signal at depth.”
One drawback of DA-OCT is its instability. “The technology right now has been kind of constrained to the benchtop. It’s a lot more intricate to align than traditional OCT, [which] is still robust,” according to Jelly. However, he says a number of clinical collaborations are underway, including the development of a handheld deep-tissue-imaging device.
“Finding a way to make the technology more robust and translational is definitely a focus,” Jelly says, “along with … finding those uses where DA might have an advantage.”